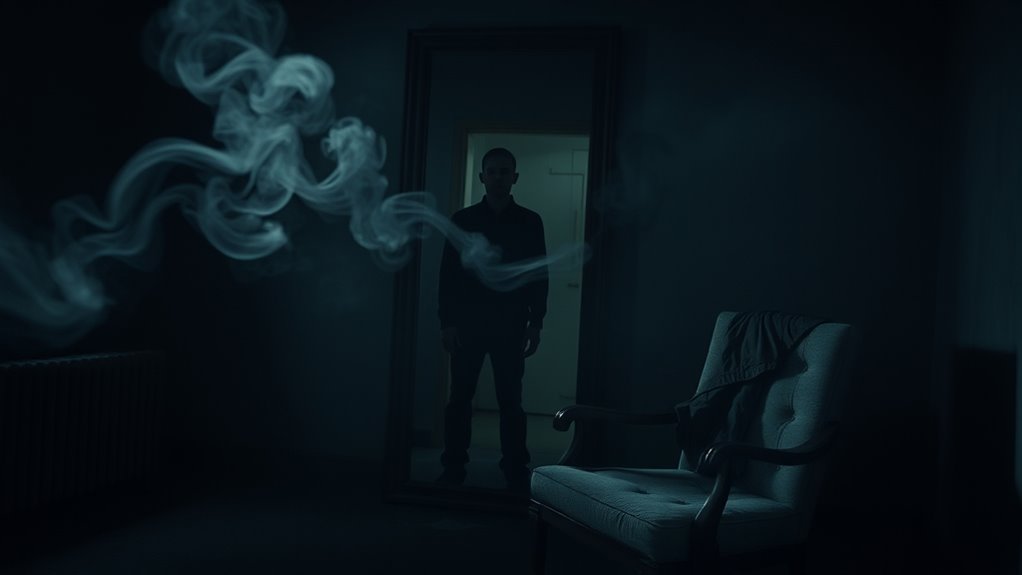
You might see things that aren’t there due to various factors affecting your perception. Neurological conditions, like dementia or epilepsy, can cause visual disturbances. Psychiatric disorders, including schizophrenia, often lead to hallucinations as well. Substance use and certain medications play a significant role too. Additionally, imbalances in brain chemicals and stress can contribute. Understanding these factors can provide clarity on your experiences, and there’s more to explore about how and why this occurs.
Key Takeaways
- Visual hallucinations can result from neurological conditions, such as epilepsy or dementia, which alter perception and cognitive function.
- Retinal diseases, like macular degeneration, disrupt visual signals and can lead to phenomena known as Charles Bonnet syndrome.
- Substance use, particularly hallucinogens, can trigger vivid hallucinations by altering neurotransmitter activity in the brain.
- Emotional crises and unresolved conflicts in psychiatric disorders, such as schizophrenia, can distort perception and lead to hallucinations.
- Prolonged sensory deprivation or stress can misattribute internal stimuli, resulting in experiences of seeing things that aren’t there.
Understanding Visual Hallucinations

When you think about visual hallucinations, it’s essential to recognize that they can stem from various causes, each affecting your perception differently. Retinal diseases can disrupt neural signals, leading to distorted images. If you suffer from migraines, you might experience auras that manifest as visual hallucinations. Prolonged visual deprivation, like blindfolding, can also trigger these experiences. Additionally, certain medications or drugs can cause visual disturbances you may not expect. Psychiatric illnesses, such as Charles Bonnet Syndrome, often introduce complex visuals influenced by psychological factors, which may be exacerbated by narcissistic behavior in interpersonal relationships. Regular skin treatments can boost skin health and may also be beneficial for individuals experiencing stress-related hallucinations. Understanding the emotional needs of individuals dealing with such experiences can also provide insight into their condition. Hallucinations can range from simple lights and colors to intricate scenes, affecting one or both eyes. Notably, the experience of angel numbers can sometimes be intertwined with these visual phenomena, reflecting deeper spiritual messages. Furthermore, engaging in spiritual practices like meditation can help individuals cope with these experiences by reducing stress and anxiety. Understanding these triggers and types is crucial for managing and addressing visual hallucinations effectively. Investigative techniques can also help in analyzing the factors contributing to these phenomena.
Neurological Conditions and Their Impact

Neurological conditions can greatly alter your perception, often leading to visual hallucinations that range from fleeting images to vivid scenes. For instance, if you have epilepsy, you might experience complex visual hallucinations during seizures due to abnormal cortical activity. Similarly, conditions like dementia often accompany cognitive decline and visual disturbances. Individuals with Borderline Personality Disorder may also struggle with emotional dysregulation, which can exacerbate perceptions and experiences. Establishing consistent daily routines can help manage some of the anxiety that leads to these experiences, as structured routines promote stability and reduce distress. Additionally, engaging in healthy meal options can support overall brain health, potentially mitigating some symptoms. Deafferentation, or loss of sensory input, can increase neuronal excitability, causing you to see things that aren’t there. In Parkinson’s disease, changes in brain activity can also lead to these experiences. Additionally, visual hallucinations are common in older individuals, highlighting the need for awareness in managing these symptoms. It is essential to recognize that narcissistic abuse can further complicate the emotional landscape, potentially intensifying these perceptual disturbances.
The Role of Psychiatric Disorders
Psychiatric disorders play a significant role in the experience of hallucinations, impacting how you perceive reality. Schizophrenia is the most common condition linked to these experiences, with over 70% of individuals encountering visual hallucinations and 60%-90% hearing voices. Early detection of these conditions is critical for effective treatment. In addition, engaging in trust-building activities can support individuals in managing their symptoms and improving their overall well-being. Understanding the impact of newborn feeding options on mental health can also provide insights into potential contributing factors. Individuals with BPD traits may also experience distortions in perception during emotional crises. Moreover, treatment approaches are evolving, with many practitioners emphasizing innovative therapies to enhance patient outcomes.
Schizoaffective disorder also includes hallucinations, while severe forms of depression and bipolar disorder can lead to them as well. Delirium, often caused by infections or drug use, may result in confusion and hallucinations.
During psychotic episodes, you might lose touch with reality, frequently experiencing these distortions. Hallucinations can vary in type, including auditory and visual, depending on the underlying psychiatric condition. Understanding these disorders is vital for effective diagnosis and treatment, which can greatly impact your quality of life. Common causes of hallucinations include conditions such as schizophrenia and Parkinson’s disease.
Substance Use and Hallucinatory Experiences

Hallucinations aren’t solely linked to psychiatric disorders; substance use also plays a significant role in these experiences. Hallucinogens can drastically alter your perception, leading to vivid hallucinations and emotional disturbances. Classic hallucinogens sometimes trigger psychotic episodes, leaving you disoriented and anxious. You might even experience unexpected flashbacks, where visual disturbances can occur long after the substance has left your system. Cold medications may sometimes exacerbate these effects, especially when combined with hallucinogenic substances. Additionally, understanding the concept of absorption rates can help clarify the relationship between substance effects and mental states. The ethical implications of utilitarianism also come into play when considering the societal impact of substance use.
Although these substances aren’t typically addictive, some users may develop a dependence over time. The risks associated with substance-induced hallucinations raise public health concerns, as they can affect both your mental and physical health. Understanding these factors is essential for anyone considering the impact of substance use on their perception of reality.
Optical Pathway Issues Contributing to Hallucinations

When visual pathways are disrupted, you may experience hallucinations that distort your perception of reality. Conditions like tumors or optic nerve damage can compress or disrupt visual signals, leading to these unsettling experiences. For instance, if you have papilledema or optic neuritis, the damage to retinal nerve fibers can create unusual visual phenomena. Additionally, individuals with macular degeneration often face Charles Bonnet Syndrome, where decreased sensory input causes increased spontaneous firing in visual brain areas, resulting in hallucinations. Up to half of individuals with macular degeneration may experience CBS, indicating that the relationship between sight loss and hallucinations is significant. Furthermore, recurring dreams of loved ones often provide a mix of emotions, offering comfort and closure and may relate to how the brain processes visual information. Maintaining a clean environment with the help of HEPA filters can reduce allergens that may exacerbate visual disturbances. It is also essential to consider the impact of dementia medications on managing symptoms associated with visual disturbances. Interestingly, disturbances in plant health can also lead to increased stress, which may influence visual perception. Effective location scouting is critical to ensure that environmental factors do not contribute to visual disturbances. Diagnostic imaging, such as MRI or CT scans, can identify structural issues along the visual pathway. Understanding these optical disruptions is essential for addressing the root causes of hallucinations and providing effective management strategies.
Psychopharmacological Factors at Play

As various substances interact with your brain’s chemistry, you might encounter vivid hallucinations that can distort your reality.
Hallucinogenic drugs like LSD and psilocybin primarily activate serotonin 5-HT2A receptors, creating intense visual and auditory distortions. Similarly, psychostimulants stimulate dopamine D2 receptors, leading to hallucinations akin to those in schizophrenia. Dissociative anesthetics, such as ketamine, block NMDA glutamate receptors, resulting in dissociative effects and hallucinations. Anticholinergic drugs like atropine can also induce hallucinations through their effects on acetylcholine pathways. Combining these substances or using certain medications, like tricyclic antidepressants, can heighten the risk of experiencing hallucinations, especially if you have pre-existing conditions. Understanding these mechanisms can help you navigate the complex world of psychopharmacology. In particular, effective communication strategies can be crucial in situations where individuals experience heightened emotional responses due to hallucinogenic effects.
In particular, visual hallucinations can also arise from neurodegenerative processes that disrupt neurotransmitter balance, contributing to the hallucinatory phenomena experienced in conditions like Parkinson’s disease.
Psychodynamic Influences on Perception

Psychodynamic influences on perception reveal how unconscious processes shape the way you interpret your experiences. Your perceptions can be distorted by unresolved conflicts and past traumas, often without your awareness. Freud emphasized that the unconscious drives behaviors, making you more prone to seeing things that aren’t there. Defense mechanisms like repression or denial can further skew reality, leading you to misinterpret situations. The interplay between your id, ego, and superego also plays an essential role; while the id seeks immediate gratification, the ego mediates between desires and reality, sometimes creating illusions. Ultimately, emotional forces from the unconscious can influence what you perceive, highlighting the complex relationship between your mind and reality. This is evident in Freud’s theory of levels of consciousness, as the unconscious may harbor repressed memories that affect perception.
Pathophysiological Mechanisms Behind Hallucinations

Hallucinations, which can feel strikingly real, often arise from complex pathophysiological mechanisms that disrupt normal brain function.
You might experience these distortions due to neurochemical imbalances, particularly with dopamine and serotonin. Glutamate dysfunction, like NMDA receptor blockade, can also contribute to these vivid experiences. In conditions such as schizophrenia, thalamocortical dysfunction leads to impaired gamma rhythm modulation, resulting in hallucinations. Additionally, sensory deprivation can induce hallucinations, even in healthy individuals. Cortical hyperexcitability, seen in Charles Bonnet syndrome, can cause visual hallucinations through deafferentation. Temporary conditions can also lead to hallucinations, particularly when factors like sleep deprivation or high fever are at play. Stress and hyperarousal play roles too, as dysregulated thalamocortical circuits can misattribute internal stimuli, making you perceive things that aren’t there.
Understanding these mechanisms sheds light on the complexity of your experiences.
Treatment Approaches for Managing Hallucinations

Finding effective treatment approaches for managing hallucinations can greatly improve your quality of life. Medications like antipsychotics, mood stabilizers, and anti-anxiety drugs are commonly prescribed to help alleviate symptoms. Psychotherapy interventions, such as Cognitive Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT), can help you address distorted thought patterns and emotional regulation. Holistic methods, including mindfulness training and yoga, can enhance overall well-being. Social support through family or group therapy also plays an essential role in reducing isolation. For more severe cases, advanced treatments like Electroconvulsive Therapy (ECT) and neurostimulation techniques are available. Approximately 21% of U.S. adults experience mental illness annually, so exploring a combination of these approaches can lead to better management of hallucinations and improve your daily functioning.
Frequently Asked Questions
Are Visual Hallucinations the Same for Everyone Who Experiences Them?
Visual hallucinations aren’t the same for everyone. You might see vivid images of animals, while someone else experiences complex scenes or figures.
Your emotions during these experiences can vary too—some feel fear, while others may find joy. The underlying causes, such as neurological conditions or psychiatric disorders, also play a role in how you perceive these hallucinations.
Can Visual Hallucinations Be a Sign of Creativity or Artistic Expression?
While some might argue that visual hallucinations are purely psychological disturbances, they can actually signify creativity and artistic expression.
When you experience these hallucinations, your mind is integrating unexpected sensory inputs, often leading to novel ideas.
Many artists have harnessed this phenomenon to challenge perceptions and create unique works.
How Do Cultural Beliefs Influence the Perception of Hallucinations?
Cultural beliefs greatly shape how you perceive hallucinations. They influence the themes and content of your experiences, whether you see religious figures or ancestral spirits.
Your social interactions and community expectations play an essential role, reinforcing these culturally specific interpretations. This means that in some cultures, you might view hallucinations as benign, while in others, they could be seen as harmful.
Understanding this cultural context is important for appropriate treatment and support.
Do Visual Hallucinations Always Indicate a Serious Underlying Condition?
Visual hallucinations can feel like you’re trapped in a surreal dream, but they don’t always mean something serious is happening.
While they can indicate conditions like dementia or schizophrenia, sometimes they’re linked to stress, migraines, or even medication side effects.
It’s essential to assess the frequency, nature, and context of these experiences.
Getting a thorough medical evaluation will help you understand what’s going on and determine the best course of action.
Can People Learn to Control Their Visual Hallucinations Over Time?
Yes, you can learn to control your visual hallucinations over time.
By practicing self-help techniques like eye movements and distraction, you may find temporary relief. Engaging in cognitive behavioral therapy can also help you develop coping strategies.
Additionally, optimizing your medications might improve your overall experience. It’s important to work closely with healthcare professionals to find the right approach tailored to your needs, enhancing your ability to manage these challenging experiences effectively.
Conclusion
In a world where reality dances with illusion, you might find yourself questioning what’s true. Hallucinations can feel as vivid as life itself, blurring the lines between perception and imagination. While neurological and psychiatric factors may cloud your vision, understanding these experiences can illuminate the path to clarity. Just as shadows flicker in the light, knowing their origins can help you navigate your mind’s complexities, transforming confusion into insight and fear into empowerment.









